CATHETER DIRECTED THROMBOLYSIS FOR DVT
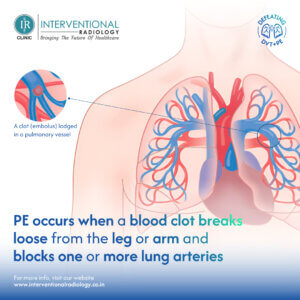
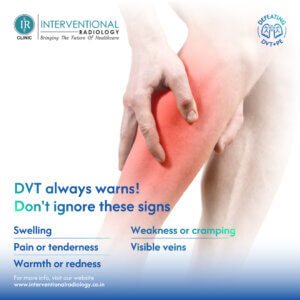
Catheter-directed thrombolysis (CDT) is a minimally invasive procedure used to treat deep vein thrombosis (DVT). DVT is a blood clot that forms in a deep vein, typically in the leg, thigh, or pelvis. If left untreated, DVT can cause serious complications, including pulmonary embolism (PE), which is a blood clot that travels to the lungs.
Procedure:
CDT involves threading a thin, flexible tube (catheter) through the bloodstream until it reaches the clot. Clot-dissolving medications, called thrombolytics, are then delivered directly to the clot through the catheter. This helps to break up the clot and restore blood flow through the vein.
Benefits:
- More effective clot removal: Compared to systemic thrombolysis (delivered through the bloodstream), CDT offers a more targeted approach. This can lead to a higher rate of clot removal and faster symptom relief.
- Reduced bleeding risk: By delivering the medication directly to the clot, CDT reduces the risk of bleeding complications compared to systemic thrombolysis.
Who is a candidate for CDT?
CDT is not suitable for everyone with DVT. Here are some factors that make a person a good candidate for CDT:
- Acute DVT: Symptoms have been present for less than two weeks.
- Proximal DVT: The clot is located in a major vein, such as the iliac or femoral vein.
- Severe symptoms: The DVT is causing significant pain, swelling, or other symptoms.
- Low bleeding risk: The person does not have any conditions that increase their risk of bleeding.
- Failure of traditional therapy: Anticoagulation medications alone haven’t been effective in resolving the clot.











IR Treatment and CDT
CDT is performed by a specially trained doctor, often an interventional radiologist (IR). IRs use imaging techniques, such as X-rays and fluoroscopy, to guide the placement of the catheter and monitor the progress of the treatment. In some cases, IRs may also use mechanical thrombectomy devices in conjunction with CDT to help remove the clot.
Things to Consider
While CDT offers advantages over traditional treatments for DVT, it’s important to be aware of some potential drawbacks:
- Bleeding risk: Although lower than systemic thrombolysis, there is still a risk of bleeding with CDT.
- Catheter complications: There is a small risk of complications associated with the insertion of the catheter, such as infection or damage to the vein.
- Length of treatment: CDT can take several hours or even days to complete.
Types of CDT:
- Low-dose CDT: This approach uses lower concentrations of thrombolytics delivered over a longer period. It’s often preferred for patients at higher risk of bleeding.
- High-dose CDT: This method utilizes higher concentrations for faster clot removal, but with a slightly increased risk of bleeding.
- Pulse spray CDT: A newer technique that delivers thrombolytics in short bursts, potentially reducing treatment time and bleeding risk.
Success Rates and Outcomes:
- Studies report successful clot removal rates ranging from 70% to 90% with CDT.
- Improved long-term outcomes include a reduced risk of post-thrombotic syndrome (PTS), a complication characterized by chronic leg pain, swelling, and skin discoloration.
- However, recent studies suggest CDT might not be significantly superior to standard anticoagulation for all patients in preventing PTS, particularly in elderly patients or those with limited clot burden.
Contraindications for CDT:
- Active bleeding or high risk of bleeding
- Recent history of stroke or intracranial hemorrhage
- Severe uncontrolled hypertension
- Pregnancy
Comparison to Interventional Radiology (IR) Treatments:
- Catheter-directed mechanical thrombectomy: This minimally invasive procedure uses specialized devices to physically remove the clot. It may be used in combination with CDT or as a standalone treatment.
- Angioplasty and stenting: In rare cases, underlying vein narrowing may contribute to DVT. IRs can perform angioplasty to open the vein and place a stent to prevent future narrowing.
The Role of Interventional Radiologists:
- Interventional radiologists are specially trained physicians with expertise in using image-guided minimally invasive procedures.
- They play a crucial role in performing CDT.
- Their skills in navigating catheters and using imaging techniques ensure accurate placement and monitor clot response to treatment.
The Future of CDT:
- Research continues to refine CDT techniques, including exploring the use of clot-busting medications specifically designed for catheter delivery.
- Optimizing treatment protocols based on individual patient characteristics is an ongoing area of focus.
Important Considerations:
- Discuss all treatment options with your doctor, including potential benefits, risks, and long-term outcomes.
- Understand that CDT is not a one-size-fits-all solution, and the best approach depends on your specific case.
- If you experience any concerning symptoms like severe pain, swelling, or bleeding after CDT, seek immediate medical attention.











