Introduction
Stroke is a leading cause of death and disability worldwide. It occurs when blood flow to a part of the brain is interrupted, depriving brain cells of oxygen and nutrients. Atherosclerosis, the buildup of fatty deposits (plaque) in the arteries, is a major risk factor for stroke. When this plaque buildup narrows arteries supplying blood to the brain (intracranial stenosis), it can significantly increase the risk of stroke.
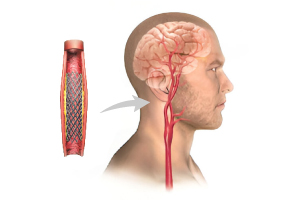
Traditionally, surgery (carotid endarterectomy) was the primary treatment for severe intracranial stenosis. However, recent advancements have introduced minimally invasive procedures like intracranial angioplasty and stenting (CAS) as alternative treatment options. This blog explores CAS, its role in stroke prevention, and the potential of interventional radiology (IR) in this field.
Intracranial Angioplasty & Stenting (CAS)
CAS is a catheter-based procedure used to widen narrowed arteries within the brain. Here’s a breakdown of the process:
- Catheterization: A thin, flexible tube (catheter) is inserted into an artery in the groin and guided through the bloodstream to the narrowed artery in the brain using X-ray imaging.
- Angioplasty: A tiny balloon attached to the catheter is inflated at the narrowed area, compressing the plaque and widening the artery to improve blood flow.
- Stenting (optional): In some cases, a small, expandable metal mesh tube (stent) is placed in the artery to hold it open and prevent future narrowing.
Benefits of CAS
Compared to traditional surgery, CAS offers several advantages:
- Minimally invasive: Minimizes surgical trauma and scarring.
- Faster recovery: Patients typically recover within a few days and can return home sooner.
- Reduced risk of complications: Less risk of bleeding and other surgical complications.
- Outpatient procedure (in some cases): May not require an overnight hospital stay.
Who is a Candidate for CAS?
CAS is not suitable for everyone. Factors influencing candidacy include:
- Severity of stenosis: The degree of narrowing in the artery.
- Location of stenosis: Location of the blockage within the brain’s vascular system.
- Patient’s overall health: Medical history and ability to tolerate the procedure.
Risks and Complications of CAS
While minimally invasive, CAS carries some potential risks, including:
- Stroke: The procedure itself can rarely cause a stroke due to blood clot formation or dislodged plaque fragments.
- Bleeding: Bleeding in the brain or groin area where the catheter is inserted.
- Allergic reaction: To contrast dye used during imaging.
Interventional Radiology (IR) in Stroke Treatment
IR plays a crucial role in CAS and other minimally invasive stroke interventions. Interventional radiologists are specially trained physicians who use image-guided procedures to diagnose and treat various conditions, including vascular diseases. They perform CAS procedures and utilize advanced imaging techniques like angiography to visualize blood flow within the brain’s arteries.
The Future of CAS and IR in Stroke Prevention
CAS is a rapidly evolving field with ongoing research to improve its effectiveness and safety. Here’s a glimpse into the future:
- Improved stent technology: Development of stents specifically designed for intracranial arteries and that reduce the risk of complications.
- Advanced imaging: Continued advancements in imaging techniques to provide even clearer visualization of blood vessels and facilitate precise stent placement.
- New treatment options: Exploring and developing other minimally invasive IR-based techniques for treating intracranial stenosis.
Intracranial Anatomy and Blood Flow
To understand CAS, let’s embark on a journey through the intricate network of blood vessels supplying the brain. The brain receives blood from two major arteries:
- Internal Carotid Artery (ICA): Located on each side of the neck, the ICA supplies blood to the front and sides of the brain. It branches further within the skull, forming the:
- Anterior Cerebral Artery (ACA): Supplying blood to the frontal and medial portions of the brain, crucial for movement, thinking, and memory.
- Middle Cerebral Artery (MCA): The most commonly affected artery in strokes, supplying blood to the lateral portions of the brain, responsible for sensation, movement, language, and vision.
- Vertebral Artery: Located on either side of the vertebral column, the vertebral arteries join to form the basilar artery at the base of the skull. The basilar artery further branches into:
- Posterior Cerebral Artery (PCA): Supplying blood to the occipital lobes at the back of the brain, responsible for vision and spatial orientation.
Intracranial Stenosis: The Culprit Behind Stroke
Atherosclerosis, the buildup of plaque within arterial walls, can narrow these vital vessels supplying the brain. This narrowing, medically termed intracranial stenosis, impedes blood flow, potentially leading to:
- Transient Ischemic Attacks (TIAs): Brief episodes (minutes to hours) of stroke-like symptoms that resolve without lasting damage. They serve as warning signs of potential future strokes.
- Stroke: When blood flow is completely blocked, brain cells die, leading to permanent neurological deficits depending on the affected brain region.
Clinical Presentation of Intracranial Stenosis
Symptoms of intracranial stenosis can vary depending on the location and severity of the blockage. However, some common presentations include:
- Weakness or numbness: This can occur on one side of the face, arm, or leg.
- Vision problems: Difficulty seeing in one or both eyes, blurred vision, or loss of vision in one half of the visual field.
- Speech difficulties: Slurred speech, difficulty finding words, or trouble understanding language.
- Balance and coordination problems: Difficulty walking, dizziness, or vertigo.
- Cognitive issues: Difficulty thinking, memory problems, or confusion.
Diagnosis of Intracranial Stenosis
Early diagnosis of intracranial stenosis is crucial for preventing strokes. Physicians typically employ various diagnostic tools:
- Medical history and physical examination: Discussing risk factors (e.g., high blood pressure, diabetes, smoking) and neurological symptoms.
- Carotid artery ultrasound (Doppler): Uses sound waves to assess blood flow velocity within the carotid arteries in the neck.
- Magnetic resonance angiography (MRA): Non-invasive imaging technique that generates detailed pictures of blood vessels using strong magnetic fields and radio waves.
- Computed tomographic angiography (CTA): Uses X-rays and contrast dye injections to create detailed 3D images of blood vessels.
- Cerebral angiography (DSA): Considered the “gold standard” for diagnosing intracranial stenosis. It involves inserting a thin catheter into an artery in the groin and threading it to the brain arteries. Contrast dye is injected, and X-ray images capture blood flow patterns, revealing blockages.
Conclusion
Intracranial angioplasty and stenting offer a promising minimally invasive approach to treat intracranial stenosis and prevent stroke. While further research is ongoing, CAS has become a valuable tool in the interventional radiologist’s arsenal for stroke management. If you have concerns about stroke risk due to narrowed arteries, consult your doctor about potential treatment options like CAS. They can assess your individual situation and determine if this procedure is a suitable approach for you.